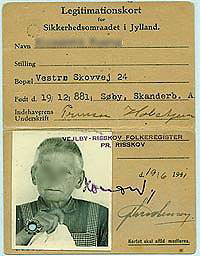
The patient NN was placed in
foster care with a family called
Koppel. She was regarded as
a family member and she lived
with them from when she was
44 years old and until she died
in 1952 at the age of 71.
When Anton Koppel retired
as a nursing assistant in 1952,
NN had to be readmitted
to the hospital after 27 years
living with the Koppel family.
However, just before this was
to happen, she died in a car
accident. Maybe she didn’t
want to be admitted again.
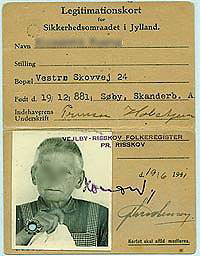
NN believed that she was a
princess. This can be seen
on her identity card, issued
in 1944, where she has signed
herself as “Princess Holstein”
Foster care at Jutland Asylum
Foster care (placing patients with a foster family as part of their care plan) was first put into use around 1900.
Incurable but stabilized patients worked for private farmers, craftsmen and widows who were living in the neighbourhood of the hospital. This form of work placement was a way of coping with increased overcrowding of the hospitals whilst at the same time being seen as a therapeutic tool.
The hospital in Risskov had an extensive family care program. From 1902 the hospital was in charge of two care centres called Dalstruup and Raamosegaard. Patients from these centres were placed in care with local families. Clothes were provided for them as well as medical supervision. The patients could live with the same family for many years and became to be considered family members. If possible the patient worked for their living. Their work could be helping in the household, in the fields or in the workshop, or it could be taking care of the children of the foster families.
One has to remember that until the 1960s there were many – now vanished – small tasks within a household. Those tasks could be emptying the stove, whitewashing and varnishing, minding chickens, sharpening tools or weaving. Laundering was a time consuming task considering that the boiler first had to be fired up before washing could begin.
New times
In the 1950s significant changes were seen in treatment of mental illness. This was largely a result of major improvement in psychotropic drugs. But also important was the abolition of family care and the fact that care staff was now public employees. Significant changes were also taking place more generally in society. Women were increasingly entering the labour market and many farms were closed down and extensive automation was seen in society. From 1956 to 1963 the number of patients in foster care was almost halved, to approx. 400, nationwide.
Psychiatry and the general hospital service
In 1953 there was a great deal of discussion about whether the big psychiatric hospitals should be closed down and whether psychiatric hospitals in the future should be located within the general hospitals.
It was by now obvious that the development of medical science – including the discovery of psychotropic drugs – opened up the possibility for beneficial collaboration with other medical specialities. In psychiatric circles there was a request for psychiatric support when a mentally ill patient was examined or treated at a general hospital. In addition, there was – over time – an economic advantage in sharing the use of costly technical equipment. There was also a desire to clarify that psychiatric treatment was in line with all other therapies. This resulted in both things continuing as before and change being implemented.
Professor Erik Strömgren, and others, argued against this plan and this resulted in both things continuing as before and change being implemented. The psychiatric hospitals were kept as they were and the general hospitals were designed to accommodate psychiatric wards.
Extensive modernisation of the large psychiatric hospitals was set into motion. Side rooms were established and numerous different activities were set into place in the wards.
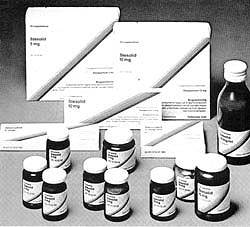
Pharmaceutical advertising in the
“American Journal of Health” 1978
for drugs to allay anxiety. Valium and
other so-called benzodiazepines were
found to be very addictive and
carried a high risk of addiction
and abuse for the person taking them.
Psychoactive drugs
P“Psychoactive drugs” is the term for medicine used in physical/biological treatment for mental illnesses. Since ancient times drugs has been used to treat mental disorders and psychological problems, drugs such as opium, hellebore and camphor.
Effective treatment
The greatest advance in psychoactive drugs was seen in 1950s where four major and crucial discoveries were made. They were to revolutionize the development of psychiatry. Now patients could be very successfully treated and the results were quite striking. This development led to an infectious optimism about such treatment, however this optimism turned out to be rather too optimistic.
This progress in the 1950s was represented in four major groups within psychoactive drugs.
Lithium: Stabilizes the mood in a manic-depressive patient.
Antipsychotics : Alleviates symptoms such as hallucinations
Antidepressants: Relieves depression and anxiety.
Benzodiazepines: Alleviates anxiety and restlessness and can induce sleep (e.g. Diazepam).
“Psychoactive drugs”, Jes Gerlach and Per Vestergaard, 1998. af Jes Gerlach og Per Vestergaard, 1998.
Within all groups with the exception of lithium many related drugs have been developed, all of them with varied patterns of effect and side effect. In recent years, for example SSR-antidepressants (Prozac) have been developed, as well as various types of medicine for side effects.
The range of side effects can be quite wide and can include nausea, headache, dry mouth, sweating, weight gain, morning fatigue, increased appetite, and disturbances in motor skills.

Average risk of developing schizophrenia amongst
relatives to people with schizophrenia – based
on studies conducted in Europe between 1920
and 1987. (Gottesman, 1991).
Heredity and environment
By studying twins and adoptees, attempts were made to discover whether mental illness (e.g. Schizophrenia) is hereditary or caused by the environment.
Is there a gene for schizophrenia or condition around upbringing that is the cause of the condition? Can a person with a gene for schizophrenia avoid getting the illness if the environment around this person is “working fine”?
Frequently occurring coincidence of mental illness in both of a pair identical twins (persons with identical genome) demonstrates how important the genetic factor is. Adopted children whose biological parents suffer from schizophrenia seem to have the same risk of developing schizophrenia whether they grow up with their ill parents or with healthy adoptive parents. This implies that hereditary predisposition plays a much greater role than the conditions around the upbringing and the environment. It is currently thought that environmental exposure only can trigger schizophrenia if there is an inherited predisposition present.
Hereditary predisposition has different impact on different mental illnesses, but many studies shows that it almost always plays a role, except where the mental illness is caused by known external or organic circumstances such as inflammation of the brain or other brain disorders, trauma to the brain , syphilis , certain vitamin deficiencies , etc.
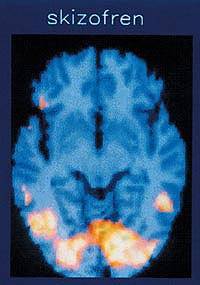
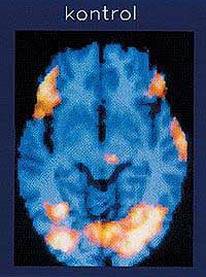
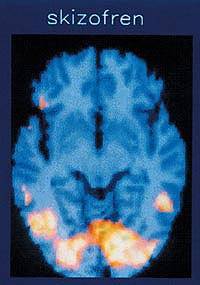
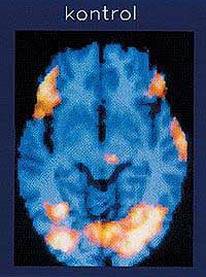
SPECT- scanning. The scanning shows the areas of the brain
(light areas) in a schizophrenic patient and a healthy patient,
where blood flow is increased during a psychological
activation
test (Wisconsin card sorting test). It clearly shows that the
schizophrenic has no activity in the frontal lobe (the sides
of the brain at the top of the pictures), while both persons
activate their sense of sight (rear, at the bottom of the
picture)– both areas showing normal activity since
both subjects have normal eyesight.
(A. Madsen, R. Hemmingsen, A. Lassen, 1996).